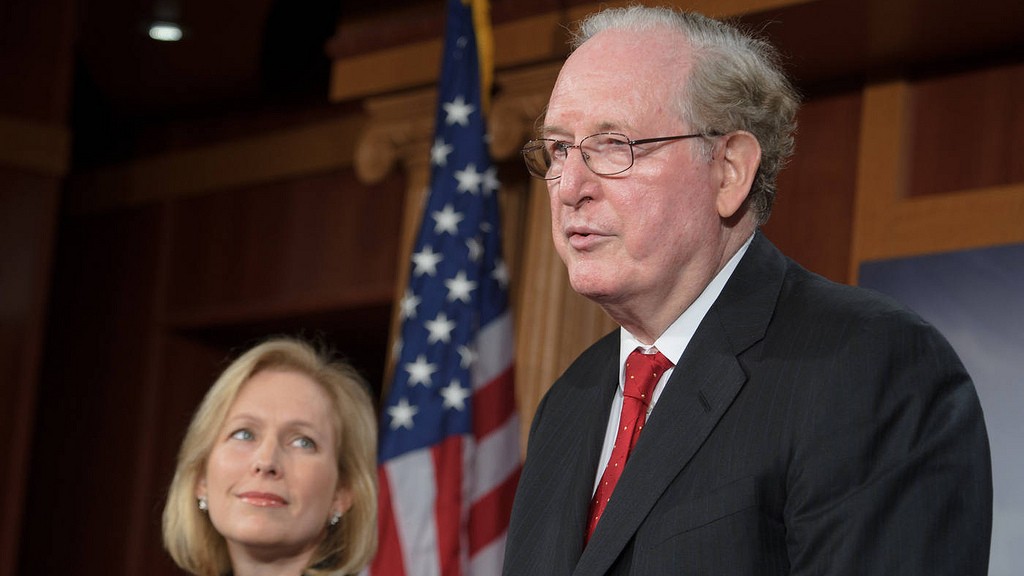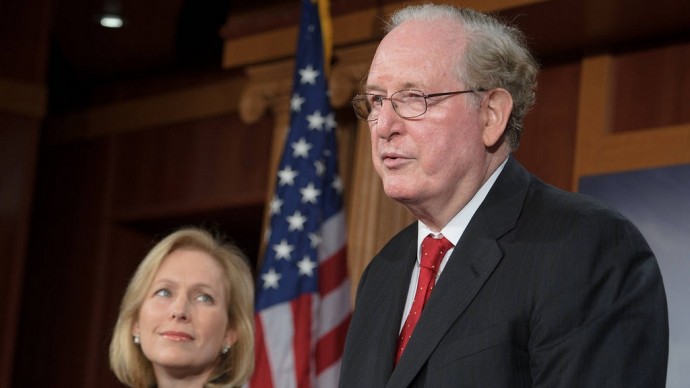
Sen. Jay Rockefeller, D-W.Va., has asked the Department of Health and Human Services to overhaul a demonstration project aimed at changing the way millions of individuals who qualify for both Medicare and Medicaid receive health care.
Finding high-quality, cost-effective ways to care for the 9 million people known as “dual eligibles” is among the brass rings of health policy. The population includes some of the sickest and poorest Americans who must navigate a fragmented system that can impede their care. Managing their care is important because it’s so costly: They account for approximately 20 percent of Medicare’s beneficiaries, for instance, but 31 percent of its spending, and 15 percent of Medicaid beneficiaries, but nearly 40 percent of that program’s spending, according to federal officials.
Twenty-six states have submitted demonstration proposals to the Centers for Medicare and Medicaid Services to integrate care for three million duals, exceeding an earlier CMS target of one to two million beneficiaries, according to the Medicare Payment Advisory Commission, which has also expressed concern about the project. The states’ proposals aim to better coordinate care and to reduce costs for both Medicare and Medicaid.
Rockefeller said that any programs testing new models of care for duals should focus on providing better care rather than saving money, especially since “some states are proposing to enroll dual eligibles in plans that have not demonstrated their ability to deliver high quality care for this population.” Rockefeller also wrote that any new care coordination ideas should be rigorously tested before they are expanded to a state’s entire population of duals, and that duals retain all the rights and the same access to care as all other Medicare beneficiaries.
HHS referred questions about the letter to CMS. In an email Wednesday, CMS spokesman Brian Cook said that the agency was “implementing important reforms that will improve care for these millions of Americans. Given the diversity and significant health care needs of dual eligibles, we recognize how critical it is to have beneficiary protections in place to achieve the highest-quality health care possible. We are taking the input from Congress, MedPAC, and others very seriously moving forward.”
In a separate letter sent Wednesday to CMS, MedPAC members said the scope of demonstrations as proposed is too broad and that only a few health plans have experience managing the full range of services that many duals need, which include medical and long-term care and behavioral health services. MedPAC urged CMS to conduct the demonstrations in a limited number of states rather than enroll millions of beneficiaries at once. The panel also recommended that beneficiaries be notified about the demonstrations and be given the chance to opt out before they are automatically enrolled in a plan that they could opt-out of later.
Sarah Barr contributed.
This story was originally published by Kaiser Health News.